Eye conditions and Treatments
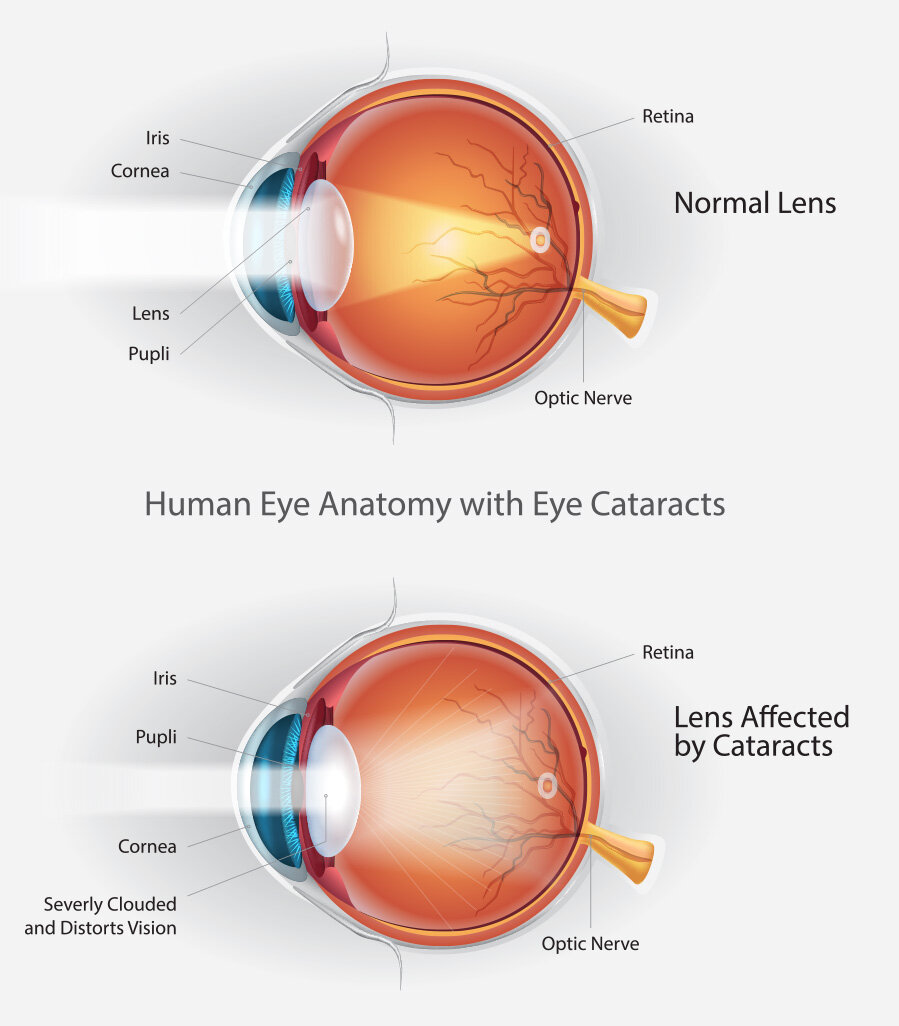
Cataract and Implant Surgery
The development of cataracts is a normal part of the aging process. In fact, it is one of the leading causes of vision loss in adults. A cataract is a clouding of the normally clear lens inside the eye. It prevents light from focusing properly on the retina. The result is blurred or out-of-focus vision, as well as the following symptoms:
Gradual blurring or hazy vision
Colors seem yellower
A tendency to become more nearsighted
Double vision in one eye only
A gradual loss of color vision
The feeling of having a film over the eyes
An increased sensitivity to glare, especially at night
When dealing with these symptoms become increasingly more difficult, and regular activities such as driving and reading are significantly impacted, it may be time to consider a cataract procedure.
The great news is that modern cataract surgery is highly successful. It can quickly restore vision and the downtime is also very minimal in most cases. Today, the surgery is a 15 minute outpatient procedure, utilizing the state-of-the-art equipment. This allows for smaller, more precise incisions, unprecedented accuracy and premier astigmatism management with NO needle and NO stitches.
Macular Degeneration
Macular degeneration is a common, acquired degenerative disease of the macula or the part of the retina needed to see objects clearly. The leading cause of blindness for people over the age of 60 in the United States, macular degeneration’s cause is still unknown. Recent studies suggest the cause may be degradation of the arteries that nourish the retina. This keeps oxygen and nutrients away from the retinal tissue. Consequently, vision deteriorates gradually and painlessly. One thing is certain, the disease runs in families, suggesting a genetic component.
There are two types of macular degeneration, dry and wet. The dry form is significantly more prevalent, with roughly 90% of patients experiencing this form of the condition. Although the wet form is only present in 10% of all people diagnosed with macular degeneration, it accounts for most of the visual loss associated with the disease. Also, with dry AMD, the loss is gradual. With wet AMD, the loss will be more rapid.
Symptoms of macular degeneration include:
Reduced central vision
Central blind spots
Visual distortion
Decreased color vision
Difficulty reading
Currently, there is no known cure for macular degeneration. Your ophthalmologist may recommend certain vitamin supplements to help control the disease. In severe cases, laser therapy or intraocular medication injections may be necessary.
If you suspect that you or a family member may have macular degeneration, please contact Cataract & Eye Consultants of Michigan as soon as possible. Our doctors and surgeons have extensive experience treating the condition, and early detection is of utmost importance. One of our ophthalmologists will dilate the eyes and inspect the retina to make a final diagnosis. If macular degeneration is detected, a special test called a fluorescein angiogram may be performed to further evaluate your retina.
If you or a loved one are diagnosed with macular degeneration, alert your ophthalmologist to any new changes in vision, especially those detected with an Amsler grid. Take the recommended vitamin supplements prescribed by your ophthalmologist. It’s also important that you never smoke, and always wear protective sunglasses when exposed to the bright sun.
Glaucoma
Glaucoma is a group of eye diseases that causes a gradual loss of vision without warning and most often without symptoms. In fact, roughly half of the 3 million Americans who have glaucoma do not realize they are affected by the disease due to the absence of warning signs. Glaucoma is the second leading cause of blindness in the U.S. and the leading cause of preventable blindness.
Vision loss from glaucoma is caused by damage to the optic nerve. The damage occurs when the pressure within the eye increases due to a build-up of fluid inside the eye. However, damage may occur without intra-ocular pressure elevation.
It is important to understand that individual response to eye pressure varies. Some people develop optic nerve damage from relatively low pressures, while others sustain no damage from higher pressures.
Open Angle Glaucoma is the most common type of the disease. Standard treatments include medication in the form of eye drops. Selective Laser Trabeculoplasty (SLT) is an advanced type of laser treatment to manage patients with Open Angle Glaucoma. SLT is a cold laser that lowers intraocular pressure by stimulating cells inside the eye to promote fluid drainage. SLT does not cause scarring inside the eye and is repeatable.
Low Tension Glaucoma is a condition where the optic nerve is damaged even though the intraocular pressure is normal. Unfortunately, everyone is at risk for glaucoma. Your risk can increase with certain factors present, including age, diabetes and a family history of glaucoma. People over 60 years of age are six times more likely to develop glaucoma.
Because Open Angle Glaucoma and Low Tension Glaucoma have no symptoms, regular eye examinations are important. Intraocular pressure measurement and careful evaluation of the optic nerve are routine elements in a comprehensive ophthalmological examination. Further testing, such as visual field testing and an optic nerve scan may be required for definitive diagnosis and follow up evaluation.
If the disease remains untreated, the optic nerve could be damaged to the point that irreversible blindness will result. Our qualified glaucoma doctors will diagnose and set a proper treatment option. Call Cataract & Eye Consultants of Michigan today for more information on how we can help with your glaucoma.
Diabetic Eye Diseases
Diabetes can cause a number of eye diseases including diabetic retinopathy, glaucoma, and cataracts, with the most common diabetic eye disease being diabetic retinopathy. It is the most common cause of blindness for people under the age of 55 in the United States. Anyone with diabetes can develop diabetic retinopathy with half of all diabetics developing some degree of diabetic retinopathy in their lifetime. Up to 80% of all patients with diabetes can be affected, and all patients with diabetes are at risk. With annual eye exams, as well as close monitoring, the disease can be prevented and controlled.
There are no symptoms in the early stages of diabetic retinopathy. People with advanced diabetic retinopathy may experience blurred vision, black floaters or sudden loss of vision. In many cases, diabetic retinopathy can be treated before vision loss occurs. This is why the American Diabetes Association recommends that all people with diabetes have a medical eye exam at least once a year. Finding and treating diabetic retinopathy early is the best way to control diabetic eye disease.
Your eye doctor can make the diagnosis of diabetic retinopathy. This requires a dilated eye exam to examine the retina is detail. The doctor will look for specific signs of diabetic retinopathy such as damaged blood vessels, hemorrhages, swelling, and abnormal growth of blood vessels. Although there is no cure for diabetic retinopathy, it is very important to control your blood sugars and blood pressures with the help of your primary doctor. At Cataract & Eye Consultants of Michigan, we have the expertise and experience necessary to diagnose and treat diabetic retinopathy.
Dry Eye
Recent studies estimate that nearly 30 million people in the U.S. suffer from dry eye disease (DED). The International Dry Eye Workshop defines the disease as follows: “Dry eye disease is a multifactorial disorder of the tears and ocular surface, associated with symptoms of discomfort, visual disturbance, and tear film instability. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.”
Our eyes need tears to stay healthy and comfortable. DED is a condition where we do not produce enough tears, or we do not produce good quality tears to properly lubricate the eyes.
Symptoms of dry eye may include:
burning/stinging eyes
gritty feeling eyes, like there is something in your eye
red, itchy or irritated eyes
intermittent blurring of vision (that may improve or change with blinking)
crusting or mucous in or around the eyes
tearing (feeling like you always have to wipe your eyes)
discomfort with contact lens use
Contributors to dry eye may include:
hormonal changes with age
eyelid conditions such as blepharitis (inflamed, crusty, red eyelids) and entropion (eyelid turning in) or ectropion (eyelid turning out)
ocular conditions such as eye allergies or prolonged contact lens wear
environmental triggers such as smoke, wind, dry climate, air conditioning/fans, makeup/makeup remover
certain daily activities result in decreased blinking such as screen time (computer, TV, cellular phone) or reading
eye surgery
certain diseases such as Sjögrens syndrome, thyroid disease, and rheumatoid arthritis
certain medications such as some blood pressure medications, allergy medications and anxiety medications
When you visit our office we will start by having you fill out a questionnaire to see how much your quality of daily life is affected by dry eye. You will have a comprehensive exam with one of our physicians, and specific diagnostic tests may be performed if needed.
Treatment focuses on targeting ocular surface inflammation, supplementing your own tears with artificial tears, and treating any contributing factors, including those mentioned above. The experienced doctors at Cataract and Eye Consultants will work with you and create a treatment plan depending on the severity of your dry eyes.
Blepharitis
Blepharitis is a chronic inflammatory condition of the eyelids and eyelashes that is characterized by an accumulation of oil, bacteria, and crusting on the eyelid margins. This condition can occur in individuals of all ages. In some people, the oil glands at the base of the eyelashes become clogged. Symptoms can include itchy eyelids, burning eyes, redness, and worsening of dry eye.
A LashCam® may be used to view the blepharitis and inflammation seen on your eyelids. If recommended by your doctor, BlephEx® treatment is available to mechanically clean your eyelids in the office by your physician.
BlephEx® is a painless in-office procedure performed by your doctor. This procedure cleans your eyelid margins, effectively removing years of accumulated bacterial biofilm, much like a dental cleaning removes accumulated plaque, also a biofilm. Once the biofilm is removed, your eyelids are cleaner and healthier. A healthy eyelid is critical for normal tear production. The procedure lasts about 6 – 8 minutes. Most patients simply report a tickling sensation. After the procedure, you may resume normal activities. BlephEx® should be repeated every 4-6 months as determined by your doctor.